Welsh Government
Designing breathing space into children’s neurodiversity services
System Thinking
Service Design
Research
2026

The challenge
Children’s neurodevelopmental services in Wales are under increasing pressure.
Demand for ADHD and autism assessments continues to rise, and waiting times remain long.
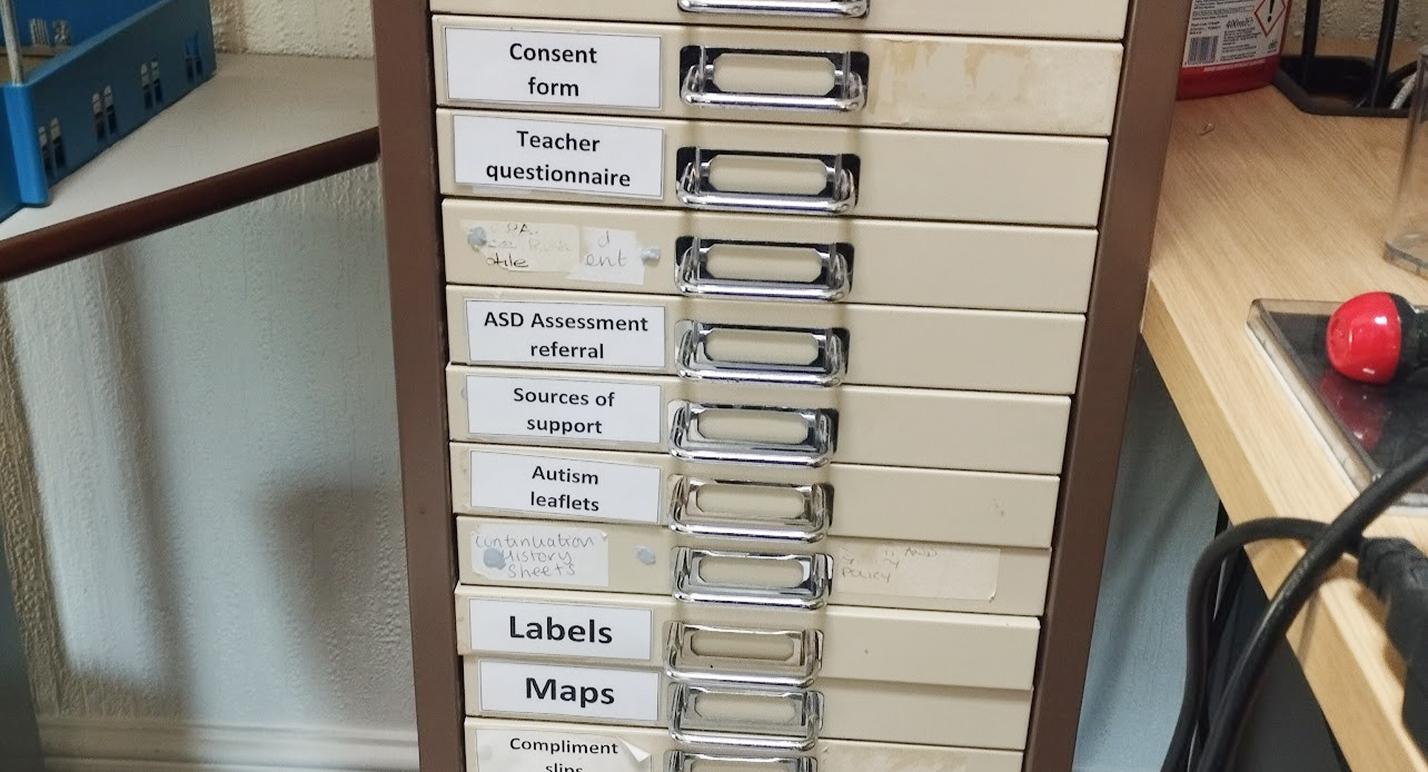
The service spans all Health Boards in Wales and involves many professional roles, systems and handovers. Clinicians are committed to delivering good care, but much of their time is spent on documentation and navigating fragmented tools.
The initial question was:
“What digital product should we introduce?”
We needed to understand the service first.
“I’ve never been part of something this impactful.”
Service Lead
Understanding the challenge
We worked across all Health Boards in Wales, spending time with the people delivering the service day to day.
Our research included:
- in-person observation of clinical practice
- interviews with clinicians, administrative staff and service leads
- workshops and site visits
- mapping the full service from referral to post-diagnostic support
This helped us see where effort was being absorbed by duplication, manual work and switching between systems — and where small changes could have a meaningful impact.
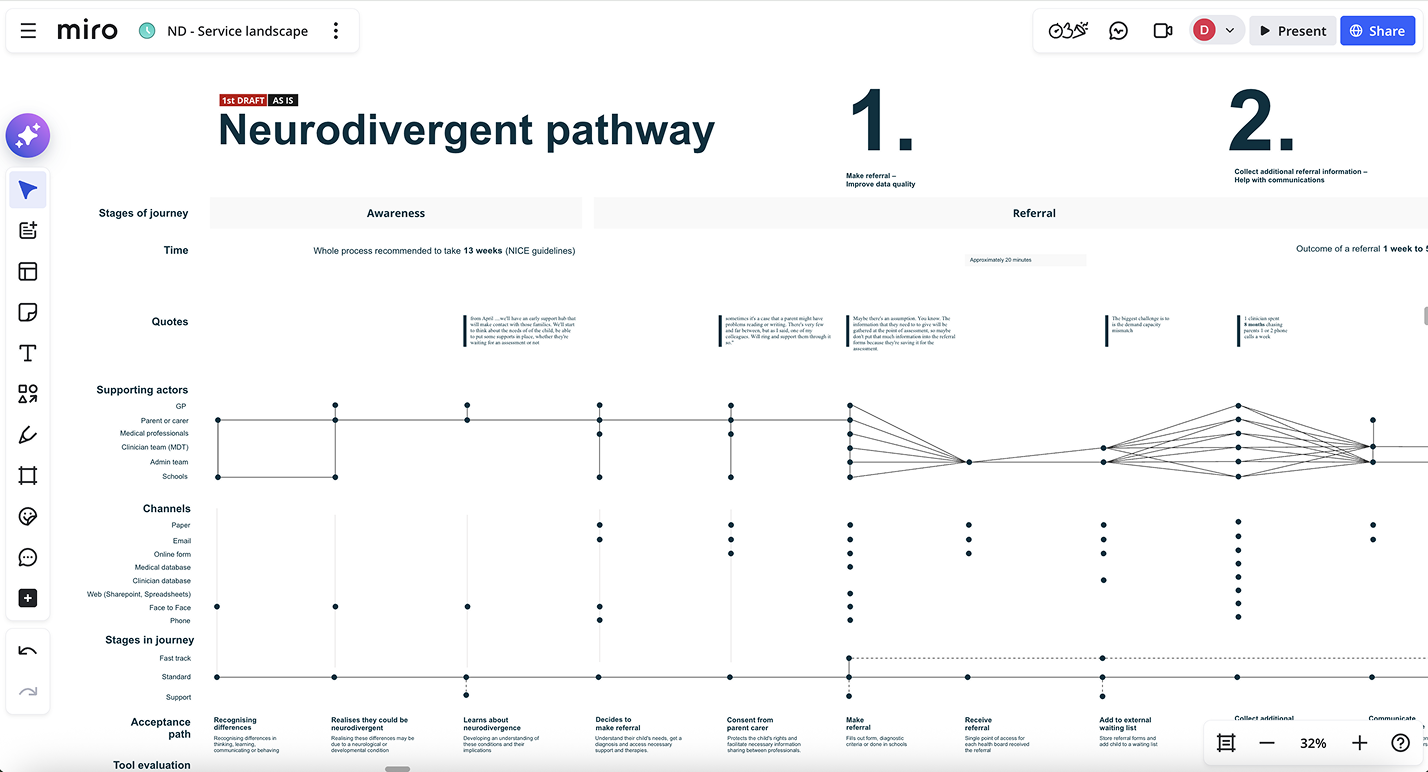
Building a shared understanding
We brought research, service maps and data together to create a shared picture of the service.
Mapping the end-to-end journey helped teams see how local decisions affected the wider system. It also shifted conversations away from individual tools and towards service flow and user needs.
We used show and tells to build trust, test assumptions and bring clinical voices into decision-making.
Shifting the approach
Instead of a requirements-led, infrastructure-heavy approach, we moved to a user-needs-led service design model.
This allowed us to focus on smaller, more impactful changes that could be tested quickly within existing systems.
We also supported a culture of continuous feedback through communities of practice, giving clinicians space to share learning and shape improvements as the work progressed.
Testing in real services
One clear opportunity was documentation.
Clinicians told us that note-taking during sessions reduced the quality of conversations and extended their working day. We designed and tested an AI scribing pilot to explore whether reducing this burden could change the experience of care.
The pilot involved:
- 5 clinicians
- around 150 hours of real clinical use
- assessments, reviews and day-to-day admin
“The family were sat down at 1.35 and the report draft was on my screen by 2.38. That would have taken me hours.”
Senior Clinician, ADHD and Autism Assessments
What we learned
The results were consistent:
- 35–80% reduction in documentation time across key activities
- reports often ready before clinicians left the room
- more natural conversations with children and families
One clinician said:
“I can have a much more natural conversation and get more clarity. It’s so helpful.”
Another shared:
“The family were sat down at 1.35 and the report draft was on my screen by 2.38. That would have taken me hours.”
A moment that mattered
During a review of the pilot dashboard, the service lead running the pilot became emotional and said:
“I’ve never been part of something this impactful.”
That moment captured the value of the work better than any metric.
Go live
The pilot results directly informed full adoption within the service.
The same approach is now being piloted in two additional Health Boards.
The focus remains on learning, iteration and supporting clinicians to deliver better care within the systems they already use.
Outcomes
- Reduced documentation time and improved clinical capacity
- Faster report turnaround for families
- More present, person-centred appointments
- A shift from large infrastructure change to targeted service improvements
- A sustainable model for continuous service learning across Wales